Measuring quality
 Ireland’s initial quality indicators for health show improvements in cardiac medicine but slower progress against stroke. eolas examines the findings.
Ireland’s initial quality indicators for health show improvements in cardiac medicine but slower progress against stroke. eolas examines the findings.
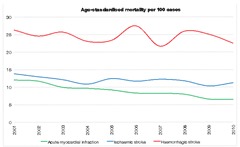
The Department of Health’s study on health care quality indicators supports the theory that outcomes for patients are better in large hospitals. It also indicates that more people are surviving cardiac arrests although it has been more difficult to reduce mortality related to strokes.
“A quality health service,” the report explains, “provides the range of services which meet the most important health needs of its population in a safe and effective way, without waste and within the regulatory framework.”
The report considers a number of indicators which could help to monitor the quality of patients’ care and the service’s overall performance. The statistical base is collated from the hospital inpatient enquiry (HIPE) system, which is managed on behalf of the Health Service Executive.
Seven potential indicators were selected. The first five monitor in-hospital mortality within 30 days of certain conditions or treatments:
• acute myocardial infarction (cardiac arrest);
• ischaemic stroke (where blood flow to the brain is interrupted);
• haemorrhagic stroke;
• hip fracture surgery; and
• emergency colectomy (removal of the large intestine).
Data were age-standardised and collected for 2008-2010 period apart from those for hip fracture surgery and colectomy (2006-2010). The other indicators covered: time to hip fracture surgery and the age at which orchidopexy is performed (to treat undescended testes).
Mortality indicators are useful for international comparisons but there is an “inevitable trade-off” with other factors which can affect their precision e.g. the presence of other medical conditions.
For the cardiac arrest indicator, mortality in Ireland almost halved between 2001 and 2010, a continuation of long-term improvements. The use of drug-based treatments has made a major difference since the 1980s.
Death rates at four Irish hospitals were 11-21 per cent above the national average. Further research found that this was explained by misdiagnoses and the cardiac arrest being a complicating factor in other major conditions.
The other 32 hospitals were close to the norm, suggesting that the improvement over the last decade has been experienced across the State.
Thrombolysis, timely diagnosis and dedicated stroke units have brought about a slight decrease in mortality for patients but the time taken to recognise symptoms and the quality of care appears to vary considerably.
Haemorrhagic stroke is less common but more fatal than ischaemic stroke. Mortality rates have varied around 25 per 100 cases over the last decade. Almost a quarter of haemorrhagic stroke cases in the study period were recorded in one large hospital, which has by far the lowest rate (12.1). The link between decreased mortality and hospital size increased reflects better expertise. The 42.4 rate recorded in one smaller hospital was particularly worrying and, in many others, a third of patients were likely to die of the condition.
Hip fracture-related mortality is relatively low and decreased from 3.4 to 2.5 per 100 cases over the 2001-2010 period. Death rates were slightly higher in smaller hospitals but again, this only accounted for a small number of fatalities which may not have been related to the surgery.
Mortality was higher in emergency colectomy cases (6.1 per 100) although the range across hospitals varied between 1.7 and 15.7. This trend was related to differences in patient age profiles.
Time-to-surgery was recorded for hip fracture patients aged 65 and over. Nationally, 79.9 per cent of patients underwent the operation within two days of admission with this figure broken down as follows:
• 30 per cent on the day of admission;
• 37.5 per cent on the following day; and
• 12.4 per cent on the second day.
 A wide variation was recorded, ranging from 95 per cent to 58 per cent within two days. The percentage of operations taking place on the day of admission had risen from 21 per cent in 2001.
A wide variation was recorded, ranging from 95 per cent to 58 per cent within two days. The percentage of operations taking place on the day of admission had risen from 21 per cent in 2001.
The authors noted that this data covers the time from admission to the ward rather than when the patient arrived in the emergency department. Hospitals with long A&E delays “may appear to be performing better than they are.”
Orchidopexy data are categorised at a regional level. Medical best practice indicates that the operation should be performed when a child is aged under two years, to prevent complications later in life.
Between 2006 and 2010, only a quarter of these operations (24.7 per cent) took place within the two-year timeframe. A further 34.3 per cent took place between the ages of two and five but the largest cohort (41 per cent) occurred after then, when the child was likely to be in school.
In the Dublin Mid Leinster area, 32.3 per cent of orchidopexies were carried in the first two years compared to 28.8 per cent in Dublin North East. The rate fell markedly to 20.4 per cent in the South area and 16.3 per cent in the West.
More research was needed to understand the underlying reasons for these trends. The problem appears to be unreported in the media due to its sensitive nature but delays can lead to infertility later in life.
Following on from the report, the Department of Health is developing a formal public national reporting system for the State. Performance indicators will be aligned – where possible – with evidence-based best practice from other countries. The indicators used in the report are viewed as a useful foundation which can be “further developed and evaluated” by the department and the HSE.
OECD comparisons
The OECD collects comparative data on mortality among people aged over 45 for cardiac arrests and strokes. The most recent figures (per 100 cases) are for 2011 or the nearest available year. Ireland’s rate for cardiac arrests (6.8) was below the average (7.9) and comparable with the Netherlands. The best performance was found in Denmark (3.0).
Ireland had one of the higher mortality rates for ischaemic stroke (9.9), similar to Australia, while the lowest are found in South Korea (3.4) and Japan (3.0). For haemorrhagic stroke, Ireland (26.2) is around the norm for the most prosperous OECD member states. Japan is again the best performer (11.8), followed by Finland (13.1).
Turkey reports that 100 per cent of hip fracture operations are carried out within two days of admission. This appears unlikely in a large and relatively poor country; the next highest performer is Iceland (95.8 per cent).





