
Waiting list numbers in the Irish healthcare system have continued their trend of reducing, but a key target for list reduction was missed in 2022. Meanwhile, the Government presses on with its pursuit of free GP care under Sláintecare, despite not having agreement with doctors’ organisations.
Waiting lists
Figures released in January 2023 showed there to be 812,016 patients on national public hospital waiting lists at the end of 2022, a 4 per cent reduction over the year. The figures also show a decrease of 3.5 per cent from October 2022, when the decrease from record levels of hospital waiting list numbers that had begun in September 2022 continued.
A record 908,519 patients were on some form of public hospital waiting lists at the end of July 2022, meaning that the December level has seen a reduction of 10.6 per cent from these record figures. Despite these reductions in the second half of 2022, the vast increases seen in the first half of the year mean that the Government has missed its target for the reduction of waiting list numbers for 2022.
Following on from the short-term Waiting List Action Plan, which delivered a 5 per cent reduction in waiting list numbers in the final quarter of 2021, the 2022 Waiting List Action Plan aimed at an 18 per cent reduction of those on active waiting lists for acute scheduled care, a total of over 132,000 people. The €350 million action plan included existing funding of €100 million for the National Treatment Purchase Fund (NTPF) for 2022, as well as an additional €50 million for NTPF activity that was expected to remove 273,000 patients from waiting lists altogether, which stood at 831,765 patients at the end of 2021. The remaining €200 million was allocated to “further increase activity so as to achieve a net reduction in waiting lists” and was spread across priority areas such as gynaecology, paediatric orthopaedics, and bariatric/obesity treatments.
Of those on the lists at the end of December 2022, over 584,600 were waiting to be seen at an outpatient clinic for the first time by a consultant, with 81,560 ‘active’ patients, defined as those waiting for an appointment for inpatient or day case treatment. Patients who have been given dates for inpatient or day case treatment are categorised separately.
Also of note was the fact that there were 58,000 patients “suspended” from waiting lists in December 2022 for various given reasons, including not being well enough to have their treatment.
Sláintecare and free GP care
The Government has signalled its intention to press ahead with the implementation of new contracts for hospital consultants, deemed a major plank of the Sláintecare reform programme, despite not having reached agreement with the various doctors’ organisations on its terms. The contract includes basic pay of between €209,915 and €252,150 per annum on a six-point scale and a 37-hour week (not including overtime) running on a schedule of 8am to 10pm on weekdays and 8am to 6pm on Saturdays. Consultants will be able to claim a maximum of €38,000 per annum for on-call duties and overtime and will also still be entitled to conduct private practice, provided that the consultant’s public commitment is complete, and the private practice occurs outside of the public hospital site.
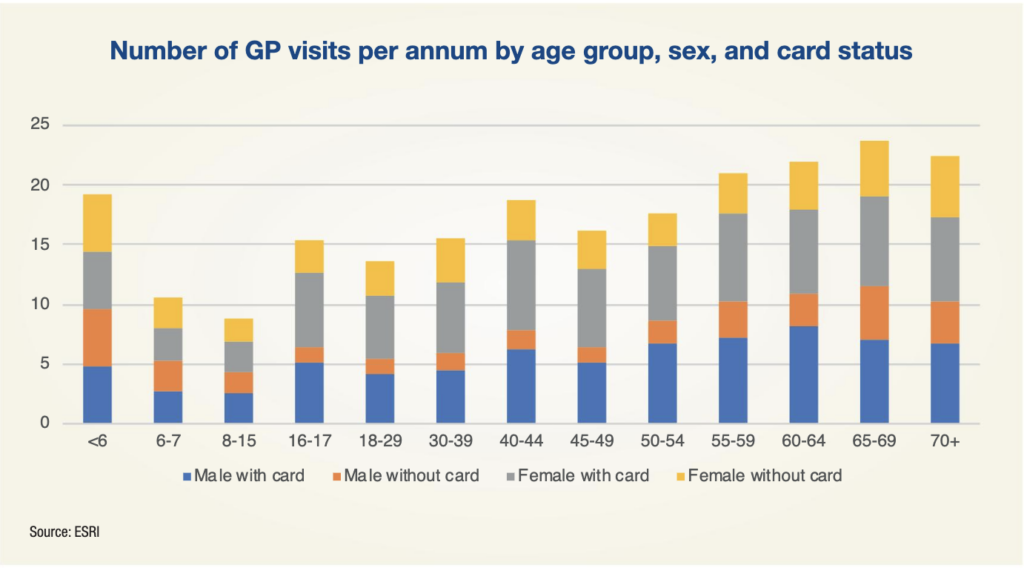
As the Government progresses through its implementation of the Sláintecare programme, research funded by the Department of Health and performed by the Economic and Social Research Institute (ESRI) shows that the implementation of free GP care to all by 2026 – another of Sláintecare’s major principles – would cost the State between €381 million and €881 million.
With 56 per cent of the population not possessing a medical card or GP visit card in 2019, the report proposes two possible scenarios for the gradual implementation of free GP care for all: age-based and income-based. In the age-based approach, it was estimated that there would be an additional 2.3 million GP visits (a 12 per cent increase) in 2026, relative to a situation of no change. The cost of this approach was estimated to range between €462 million and €881 million.
An income-based approach, whereby the income threshold for a GP visit card would be extended in 2024, 2025, and 2026 to cover approximately one-third of non-cardholders each year, would cost between €381 million and €881 million, with this lower possible cost “due to the assumption of a lower uptake rate under this approach”.
Cost estimates were found to be particularly sensitive to both take-up and payment to GP rates: an example used in the report states that reducing the payment per visit rate to GPs to 75 per cent of its current level would decrease projected costs by between 10 and 17 per cent, while increasing the payment to 135 per cent of its current level would increase costs by between 27 and 31 per cent. The costs to the State for new cardholders was found to be “relatively insensitive to assumptions on population growth”.
The projected cost to the State for existing cardholders in 2026 was between €779 million and €1.058 billion. The introduction of free GP care was estimated to decrease out-of-pocket expenditure on GP services in 2026 by between €467 million and €95 million (in an age-based scenario) or €161 million (in an income-based scenario).
The challenge facing the Government in this implementation will be convincing those who will deliver the care – GPs – that it is in their best interests, with Denis McCauley, Chairman of the Irish Medical Organisation’s GP Committee, telling RTÉ’s Morning Ireland show that he did not “recognise those figures” with regard to the ESRI’s estimate of people likely to avail of free GP care. “I worry greatly about this. It does not matter what policy is there, it is the capacity to follow it that matters,” he said.
“A plan to expand free GP care will overwhelm the system which is already dysfunctional.”
Irish College of General Practitioners representatives told the Oireachtas health committee in December 2022 that roughly 1,800 more GPs are required to staff increasing demand caused by the expansion of free care, which would take the total to approximately 6,000, an equivalent of 4,000 full-time roles. Those figures are currently standing at 4,250 and 2,800 respectively; it will fall upon the Government to ensure recruitment is done to a level that guarantees the successful implementation of its Sláintecare reforms.





